Leads ECG Placement: 7 Critical Mistakes You Must Avoid Now
Understanding the correct leads ecg placement is essential for accurate cardiac monitoring and diagnosis. A small error in electrode positioning can lead to misinterpretation of heart rhythms, potentially resulting in incorrect treatment. In this comprehensive guide, we’ll explore every aspect of leads ecg placement to ensure precision, reliability, and patient safety.
Understanding the Basics of Leads ECG Placement

Before diving into advanced techniques and troubleshooting, it’s crucial to understand the fundamental principles behind leads ecg placement. This process involves positioning electrodes on the patient’s body to record the electrical activity of the heart from multiple angles. The standard 12-lead ECG uses ten electrodes—four on the limbs and six on the chest—to generate twelve different views of the heart’s electrical function.
What Are ECG Leads and Why They Matter
ECG leads are not physical wires but rather electrical perspectives created by measuring voltage differences between electrodes. Each lead provides a unique view of the heart’s depolarization and repolarization cycles. Accurate leads ecg placement ensures that these views are consistent and clinically meaningful.
- There are limb leads (I, II, III, aVR, aVL, aVF) and precordial (chest) leads (V1–V6).
- Limb leads assess the heart’s electrical activity in the frontal plane.
- Precordial leads provide information about the horizontal plane, particularly the left ventricle.
“The ECG is only as good as the electrode placement” — Dr. Philip J. Podrid, renowned cardiologist and ECG educator.
Anatomy and Physiology Behind Lead Placement
The heart’s electrical system begins in the sinoatrial (SA) node, spreads through the atria, passes the atrioventricular (AV) node, and travels down the bundle of His and Purkinje fibers. Leads ecg placement must align with anatomical landmarks to capture this sequence accurately.
- The intercostal spaces, particularly the 4th and 5th, are critical for chest lead positioning.
- The right and left arm electrodes establish the baseline electrical reference points.
- Incorrect placement can mimic pathologies like myocardial infarction or arrhythmias.
Standard 12-Lead ECG Electrode Positions
Proper leads ecg placement follows internationally recognized guidelines set by organizations such as the American Heart Association (AHA) and the European Society of Cardiology (ESC). These standards ensure consistency across healthcare settings and facilitate accurate interpretation by clinicians.
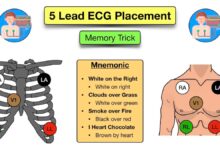
Limb Lead Placement: Arms and Legs
Limb leads are derived from electrodes placed on the right arm (RA), left arm (LA), right leg (RL), and left leg (LL). While the exact location on the limbs can vary, they should be placed distally—on the wrists and ankles—to minimize interference from muscle activity.
- RA electrode: Right wrist or upper inner forearm.
- LA electrode: Left wrist or upper inner forearm.
- RL electrode: Right ankle or lower inner leg (ground electrode).
- LL electrode: Left ankle or lower inner leg.
It’s important to note that while limb electrodes can be placed on the torso in certain situations (e.g., amputations), this alters the lead vectors and must be documented.
Chest (Precordial) Lead Placement: V1 to V6
The chest leads are placed in specific intercostal spaces along defined anatomical landmarks. Misplacement by even one intercostal space can significantly alter ECG readings.
- V1: 4th intercostal space, right sternal border.
- V2: 4th intercostal space, left sternal border.
- V3: Midway between V2 and V4.
- V4: 5th intercostal space, midclavicular line.
- V5: Same horizontal level as V4, anterior axillary line.
- V6: Same horizontal level as V4 and V5, midaxillary line.
For women, V4–V6 should be placed below the breast tissue when possible to avoid signal attenuation. In obese patients or those with large breasts, special attention is required to locate anatomical landmarks accurately.
Common Errors in Leads ECG Placement
Despite standardized protocols, errors in leads ecg placement are surprisingly common. Studies show that up to 50% of ECGs may have some degree of incorrect electrode positioning, leading to diagnostic inaccuracies.
Misplaced Chest Leads: The Most Frequent Mistake
One of the most prevalent errors is incorrect placement of precordial leads, especially V1 and V2. Placing them in the 3rd or 5th intercostal space instead of the 4th can mimic anterior myocardial infarction patterns.
- V1 and V2 too high: Can mimic anteroseptal infarction.
- V1 and V2 too low: May mask true ST-segment changes.
- Lateral leads (V4–V6) not aligned horizontally: Creates false rotation patterns.
A study published in Circulation found that even experienced technicians occasionally misplace V4, leading to misdiagnosis in emergency settings.
Reversed Limb Electrodes: A Dangerous Oversight
Reversing the right and left arm electrodes is a classic error that dramatically alters the ECG. This mistake causes lead I to invert, and leads II and III to switch, potentially mimicking dextrocardia or complex arrhythmias.
- Lead I becomes negative; P waves, QRS complexes, and T waves are inverted.
- Extreme axis deviation may be falsely interpreted.
- Can delay diagnosis of acute coronary syndromes.
“A reversed arm lead can make a normal ECG look like a life-threatening condition” — Clinical Electrocardiography: A Simplified Approach.
Impact of Incorrect Leads ECG Placement on Diagnosis
Inaccurate leads ecg placement doesn’t just produce a messy tracing—it can directly impact clinical decision-making. Diagnostic errors due to poor electrode positioning are a significant but often overlooked source of patient harm.
Mimicking Myocardial Infarction
One of the most dangerous consequences of misplaced leads is the false appearance of ST-segment elevation or depression, which can be mistaken for acute myocardial infarction.
- High placement of V1–V2 can create QS complexes resembling anteroseptal MI.
- Lateral lead misplacement may simulate lateral wall ischemia.
- Reversed arm leads can mimic inferior MI patterns.
This can lead to unnecessary activation of cardiac catheterization labs, increased healthcare costs, and patient anxiety.
Altering Axis and Chamber Enlargement Interpretation
The electrical axis of the heart is calculated using the limb leads. If electrodes are misplaced, the axis can appear deviated when it is not.
- Left axis deviation may be falsely diagnosed due to limb lead reversal.
- Right axis deviation can be mimicked by poor chest lead alignment.
- Criteria for left ventricular hypertrophy (LVH) may be met falsely due to altered R-wave progression.
These misinterpretations can lead to inappropriate referrals for echocardiography or other imaging studies.
Best Practices for Accurate Leads ECG Placement
To ensure diagnostic accuracy, healthcare providers must adhere to best practices in leads ecg placement. These include proper patient preparation, anatomical landmark identification, and continuous education.
Patient Preparation and Skin Assessment
Before placing electrodes, the skin should be cleaned and prepared to reduce impedance and improve signal quality.
- Shave excessive chest hair if necessary.
- Clean the skin with alcohol wipes to remove oils and dead skin cells.
- Lightly abrade the skin with gauze if signal noise is high.
For patients with diaphoresis or oily skin, additional adhesive pads or fixation methods may be needed.
Step-by-Step Guide to Correct Placement
Follow this systematic approach to ensure accurate leads ecg placement every time:
- Position the patient supine or semi-reclining, arms at sides.
- Locate the sternal angle (angle of Louis) at the 2nd rib.
- Move down to the 4th intercostal space for V1 and V2.
- Find the 5th intercostal space at the midclavicular line for V4.
- Place V3 midway between V2 and V4.
- Align V5 and V6 horizontally with V4 at the anterior and midaxillary lines.
- Attach limb electrodes on wrists and ankles, avoiding bony prominences.
Double-check all positions before initiating the recording. Use anatomical landmarks, not previous marks, as reference points.
Special Considerations in Leads ECG Placement
Certain patient populations and clinical scenarios require modifications to standard leads ecg placement protocols. These adaptations ensure diagnostic accuracy while maintaining patient comfort and safety.
Placement in Women and Obese Patients
Accurate leads ecg placement in women and obese individuals presents unique challenges due to breast tissue and body habitus.
- Ask female patients to reposition their breasts to locate the 5th intercostal space accurately.
- Place V4–V6 on the chest wall beneath the breast, not on the breast tissue itself.
- Use longer lead wires or extensions if necessary.
- In obese patients, ultrasound guidance may help identify intercostal spaces.
A study in European Heart Journal – Cardiovascular Imaging suggests that up to 30% of ECGs in obese patients have inaccurate V4 placement due to difficulty palpating landmarks.
ECG in Pediatric and Neonatal Patients
While the lead positions are similar, pediatric ECGs require smaller electrodes and careful attention to body proportions.
- Use pediatric-sized electrodes to ensure good contact.
- Place chest leads according to anatomical landmarks, not fixed distances.
- In neonates, the heart is more horizontal, affecting R-wave progression.
- Document any deviations from standard placement.
Pediatric ECG interpretation also differs due to age-related changes in heart rate, axis, and waveform morphology.
Technological Advances and Future of Leads ECG Placement
As technology evolves, new tools are emerging to improve the accuracy and consistency of leads ecg placement. These innovations aim to reduce human error and enhance diagnostic reliability.
Digital Guidance Systems and Wearable Sensors
Some modern ECG machines now include visual or audio feedback systems to guide electrode placement.
- Augmented reality (AR) apps overlay correct lead positions on a patient’s body via smartphone or tablet.
- Wearable ECG patches with pre-configured lead layouts reduce placement errors.
- AI-powered systems analyze real-time signals to detect misplacement.
For example, the Cardiac Science G5 ECG system includes placement verification software that alerts technicians to potential errors.
Machine Learning in ECG Interpretation
Artificial intelligence is being trained to recognize patterns of lead misplacement and correct them algorithmically.
- Deep learning models can detect reversed limb leads with over 90% accuracy.
- Some systems automatically adjust the display to show a “corrected” ECG.
- Future devices may integrate anatomical scanning to guide placement.
While promising, these technologies are not yet a substitute for proper training and technique.
Training and Education for Healthcare Providers
Despite the availability of guidelines, ongoing education is essential to maintain high standards in leads ecg placement. Many errors stem from inadequate training or lack of refresher courses.
Simulation-Based Learning and Competency Assessment
Simulation labs allow trainees to practice leads ecg placement on mannequins with real-time feedback.
- Use of ECG simulators that generate tracings based on lead position.
- Video-based assessments to evaluate technique.
- Regular competency checks for ECG technicians and nurses.
Institutions like the Advanced Cardiac Life Support (ACLS) program now include lead placement modules in their certification courses.
Standardization Across Healthcare Facilities
Hospitals and clinics should establish standardized protocols and visual aids for leads ecg placement.
- Post anatomical diagrams in ECG rooms.
- Use color-coded electrodes and lead wires.
- Implement checklists for ECG acquisition.
Standardization reduces variability and improves inter-rater reliability, especially in multi-provider environments.
What happens if ECG leads are placed incorrectly?
Incorrect leads ecg placement can lead to misdiagnosis, including false signs of myocardial infarction, axis deviation, or chamber enlargement. It may result in unnecessary tests, treatments, or missed diagnoses, compromising patient safety.
How can I verify correct ECG lead placement?
You can verify placement by checking anatomical landmarks, ensuring V1 and V2 are in the 4th intercostal space, V4 at the 5th ICS midclavicular line, and all lateral leads are horizontally aligned. Some modern ECG machines offer placement validation features.
Can limb leads be placed on the torso?
Yes, in cases of amputations or severe limb injuries, limb leads can be placed on the torso (called “alternative” or “proximal” placement), but this must be clearly documented as it alters the ECG appearance and interpretation.
Why is V4 placement so important in leads ecg placement?
V4 is a key reference point for the left ventricle. Its correct placement at the 5th intercostal space in the midclavicular line ensures accurate assessment of anterior and lateral wall activity. Misplacement can distort R-wave progression and mimic ischemia.
Are there differences in leads ecg placement for men and women?
The anatomical positions are the same, but in women, chest leads V4–V6 should be placed beneath the breast tissue on the chest wall, not on the breast itself, to ensure accurate signal transmission and avoid artifact.
Accurate leads ecg placement is a cornerstone of reliable cardiac diagnosis. From understanding the basic anatomy to avoiding common errors and embracing technological advancements, every step in the process matters. By following standardized protocols, continuously educating healthcare providers, and utilizing modern tools, we can significantly reduce diagnostic errors and improve patient outcomes. Remember, the quality of an ECG is only as good as the precision of its lead placement—so take the time to get it right every single time.
Further Reading: