Leads on ecg: 7 Leads on ECG: Ultimate Guide to Mastering Heart Diagnostics
Ever wondered how doctors decode the secrets of your heart with just a few squiggly lines? It all starts with understanding the 7 leads on ECG that capture your heart’s electrical activity from different angles—each one a vital clue in diagnosing cardiac health.
Understanding the Basics of Leads on ECG

Electrocardiography, commonly known as ECG or EKG, is a non-invasive diagnostic tool used to record the electrical activity of the heart. At the heart of this technology—pun intended—are the leads on ECG, which are essentially different perspectives or views of the heart’s electrical impulses. These leads help clinicians assess rhythm, detect ischemia, identify arrhythmias, and evaluate overall cardiac function.
What Are Leads on ECG?
In ECG terminology, a “lead” refers to a specific combination of electrodes placed on the body that measures the voltage difference between two or more points. Despite common misconception, a lead is not the same as an electrode. While electrodes are the physical sensors attached to the skin, leads are the electrical pathways created by connecting these electrodes in various configurations.
For example, Lead I measures the voltage difference between the right and left arms. This allows the ECG machine to generate a waveform that represents the heart’s depolarization and repolarization cycles from that particular angle. The standard 12-lead ECG uses 10 electrodes to produce 12 different leads—each offering a unique vantage point.
Types of Leads: Limb vs. Precordial
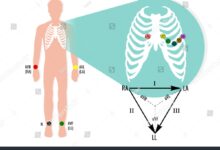
The 12 leads in a standard ECG are divided into two main categories: limb leads and precordial (chest) leads. The limb leads (I, II, III, aVR, aVL, aVF) provide views of the heart in the frontal plane, while the precordial leads (V1–V6) offer horizontal plane perspectives.
- Limb Leads: Placed on arms and legs, they form the basis of Einthoven’s triangle.
- Precordial Leads: Positioned across the chest, they capture anterior, lateral, and septal activity.
- Augmented Limb Leads: aVR, aVL, and aVF are unipolar leads derived mathematically to enhance signal clarity.
Understanding these distinctions is crucial when interpreting leads on ecg for accurate diagnosis. For more detailed information, visit the American Heart Association.
“The ECG is one of the most powerful diagnostic tools in cardiology—when interpreted correctly, it can save lives.” — Dr. Eugene Braunwald, Harvard Medical School
The 12-Lead ECG System Explained
While the title mentions ‘7 leads on ECG,’ the standard clinical practice involves a 12-lead system. However, subsets of these leads—such as the 7 most commonly analyzed—are often emphasized in emergency and educational settings. Let’s break down how the full 12-lead system works and why certain leads are prioritized.
Standard Limb Leads (I, II, III)
These three leads form Einthoven’s triangle, named after Willem Einthoven, who invented the ECG. Each lead measures electrical flow between two limbs:
- Lead I: Right arm to left arm
- Lead II: Right arm to left leg
- Lead III: Left arm to left leg
Lead II is particularly important because it aligns closely with the heart’s primary electrical axis, making it ideal for monitoring rhythm and detecting inferior wall myocardial infarctions. In fact, many bedside monitors use Lead II as the default due to its clear P-wave visibility.
Augmented Limb Leads (aVR, aVL, aVF)
These are unipolar leads, meaning they use a single positive electrode with a combined reference from the other two limbs. Though less intuitive, they provide critical additional views:
- aVR: Looks at the heart from the right shoulder—often reciprocal in nature.
- aVL: Focuses on the high lateral wall.
- aVF: Views the inferior wall, similar to Lead II and III.
aVR is often overlooked, but it can be a game-changer in diagnosing global ischemia or dextrocardia. For instance, a significantly positive QRS complex in aVR may indicate severe widespread injury.
Positioning and Placement of Leads on ECG
Accurate interpretation of leads on ecg begins with correct electrode placement. Even minor deviations can lead to misdiagnosis, such as falsely indicating myocardial infarction or arrhythmia. The American Heart Association (AHA) and other international bodies have standardized guidelines for lead positioning.
Electrode Placement for Limb Leads
Limb electrodes should be placed on the wrists and ankles, preferably on the fleshy parts rather than directly over bony prominences. This reduces motion artifact and improves signal quality. The standard color coding is:
- RA (Right Arm): White
- LA (Left Arm): Black
- RL (Right Leg): Green (ground)
- LL (Left Leg): Red
It’s essential to ensure that the patient is relaxed and lying flat to minimize interference. Incorrect placement—such as swapping RA and LA—can invert leads I, aVL, and aVR, leading to diagnostic errors.
Precordial Lead Placement (V1–V6)
The chest leads are placed in specific intercostal spaces along the thorax:
- V1: 4th intercostal space, right sternal border
- V2: 4th intercostal space, left sternal border
- V3: Midway between V2 and V4
- V4: 5th intercostal space, midclavicular line
- V5: Anterior axillary line, same horizontal level as V4
- V6: Midaxillary line, same level as V4
Errors in V1/V2 placement are common and can mimic anterior myocardial infarction. A study published in NCBI found that up to 40% of ECGs have misplaced precordial leads, emphasizing the need for training and vigilance.
“Proper lead placement isn’t just technical detail—it’s the foundation of diagnostic accuracy.” — Journal of Electrocardiology
Interpreting Key Leads on ECG for Clinical Diagnosis
Not all leads on ecg are used equally in every situation. Clinicians often focus on a core set of 7 leads—II, III, aVF, V1, V2, V5, and V6—because they provide comprehensive coverage of the heart’s major regions. Let’s explore how these leads guide diagnosis.
Identifying Inferior Wall Myocardial Infarction
Leads II, III, and aVF are the primary leads for detecting inferior wall MI. ST-segment elevation in two or more of these leads suggests occlusion of the right coronary artery (RCA) or left circumflex artery (LCx).
- Concomitant ST elevation in III > II suggests RCA involvement.
- ST elevation in II > III may point to LCx occlusion.
- Reciprocal changes in aVL (ST depression) further support the diagnosis.
Additionally, right-sided leads (V4R) may be used if suspicion for right ventricular infarction is high, especially in patients with hypotension and clear lung fields.
Diagnosing Anterior and Septal Myocardial Infarction
V1–V4 are critical for identifying anterior and septal damage. ST elevation in V1–V3 often indicates occlusion of the left anterior descending (LAD) artery, sometimes called the “widow-maker” due to its high mortality risk.
- V1 and V2: Septal region
- V3 and V4: Anterior wall
- Loss of R-wave progression across V1–V4 may indicate prior infarction.
In some cases, posterior MI can be inferred from tall R waves and ST depression in V1–V3, prompting the use of posterior leads (V7–V9) for confirmation.
The Role of Lead I and aVL in Lateral Wall Assessment
While often grouped with inferior leads, Lead I and aVL are pivotal for evaluating the lateral wall of the left ventricle. These leads are particularly useful in identifying high lateral myocardial infarctions.
Lead I: The Horizontal Plane Indicator
Lead I runs horizontally from right to left, making it sensitive to lateral wall activity. ST elevation in Lead I, especially when accompanied by changes in aVL and V5–V6, suggests lateral MI, typically due to occlusion of the left circumflex or diagonal branches of the LAD.
It’s also essential in axis determination. A positive QRS in Lead I indicates normal or left axis deviation, while negativity suggests right axis deviation or possible dextrocardia.
aVL: The High Lateral Sentinel
aVL complements Lead I by providing a more superior view of the lateral wall. In acute MI, ST elevation in aVL with reciprocal changes in II, III, and aVF can indicate a high lateral infarct.
- Isolated ST elevation in aVL is rare but can occur in early stages.
- Always correlate with clinical symptoms and troponin levels.
- Consider posterior involvement if V1–V3 show ST depression.
Recent guidelines from the American College of Cardiology emphasize the importance of aVL in risk stratification for acute coronary syndromes.
Special Considerations: Right-Sided and Posterior Leads
While the standard 12-lead ECG covers most clinical scenarios, certain conditions require extended lead sets. Right-sided and posterior leads are not part of routine screening but are invaluable in specific cases involving right ventricular or posterior infarction.
Right-Sided ECG (V4R)
When inferior MI is diagnosed, especially with hemodynamic instability, placing a right-sided lead (V4R) over the right chest can detect right ventricular involvement. ST elevation in V4R is a strong predictor of RCA occlusion proximal to the right ventricular branch.
- V4R placement: 5th intercostal space, midclavicular line on the right side.
- Positive V4R ECG has high specificity for RV infarction.
- Treatment differs—fluids are often needed instead of nitrates, which can cause collapse.
According to a study in the Journal of the American College of Cardiology, early recognition of RV infarction via V4R can reduce mortality by guiding appropriate fluid resuscitation.
Posterior Leads (V7–V9)
Posterior MI is often missed because standard leads don’t directly view the back of the heart. However, clues like ST depression and tall R waves in V1–V3 may prompt the use of posterior leads.
- V7: Left posterior axillary line
- V8: Left scapular line
- V9: Left paraspinal area
ST elevation in V7–V9 confirms posterior MI, usually due to circumflex or RCA dominance. These leads are especially useful in young patients with atypical presentations.
“Posterior MI is a silent killer—only visible with extended leads.” — Dr. Tomas Garcia, Mayo Clinic
Common Errors and Pitfalls in Using Leads on ECG
Even experienced clinicians can fall prey to misinterpretation when dealing with leads on ecg. Errors range from technical issues to cognitive biases. Recognizing these pitfalls is key to avoiding diagnostic disasters.
Lead Misplacement and Its Consequences
As mentioned earlier, misplaced electrodes are a leading cause of ECG misinterpretation. Common errors include:
- Swapping left and right arm electrodes: Inverts Lead I and affects aVL/aVR.
- Placing V4 too high or low: Alters R-wave progression.
- Incorrect intercostal space: V1/V2 placed at 2nd or 3rd space can mimic anterior MI.
A 2018 study in Heart Rhythm found that 35% of ECGs in emergency departments had at least one lead placement error. Always double-check positioning before interpreting.
Electrical Interference and Artifacts
External factors like muscle tremors, poor electrode contact, or electrical interference can distort waveforms. These artifacts may mimic arrhythmias such as atrial fibrillation or ventricular tachycardia.
- 60-cycle interference: Appears as fine oscillations, common in ungrounded equipment.
- Wandering baseline: Caused by poor skin contact or patient movement.
- Respiratory variation: Can mimic ST changes if not recognized.
Always correlate ECG findings with the patient’s clinical status. Repeat the ECG if artifacts are suspected.
Advanced Applications of Leads on ECG in Modern Medicine
With advances in technology, the use of leads on ecg has expanded beyond traditional diagnostics. From AI-assisted interpretation to wearable monitors, ECG leads are evolving to meet modern healthcare demands.
AI and Machine Learning in ECG Interpretation
Artificial intelligence is revolutionizing how we analyze leads on ecg. Algorithms can now detect subtle patterns invisible to the human eye, such as early signs of hypertrophic cardiomyopathy or low ejection fraction.
- Apple Watch ECG uses a single lead (similar to Lead I) to detect atrial fibrillation.
- Google Health has developed AI models that predict cardiovascular risk from retinal scans and ECG data.
- Deep learning models can classify MI with over 90% accuracy using 12-lead inputs.
A landmark study published in Nature Medicine demonstrated that AI could predict patient mortality from ECG data alone, even when the ECG was interpreted as “normal” by cardiologists.
Portable and Wearable ECG Devices
Devices like the KardiaMobile, AliveCor, and Zio Patch allow patients to record ECGs at home using fewer leads. While not replacing the 12-lead ECG, they provide valuable data for arrhythmia monitoring.
- Single-lead ECGs: Useful for rhythm screening (e.g., AFib).
- Long-term monitoring: Patches can record for up to 14 days.
- Remote transmission: Enables real-time cardiologist review.
These innovations democratize cardiac monitoring, especially in rural or underserved areas.
What do the 12 leads on ECG represent?
The 12 leads on ECG represent 12 different electrical views of the heart. Six limb leads (I, II, III, aVR, aVL, aVF) view the heart in the frontal plane, while six precordial leads (V1–V6) provide horizontal plane views. Together, they allow comprehensive assessment of cardiac electrical activity.
Which leads on ECG show anterior MI?
Anterior myocardial infarction is best seen in precordial leads V1 to V4. ST-segment elevation in these leads suggests damage to the anterior wall of the left ventricle, often due to occlusion of the left anterior descending (LAD) artery.
Why is Lead II commonly used in monitoring?
Lead II is commonly used in cardiac monitoring because it aligns well with the heart’s electrical axis, providing a clear view of P waves and QRS complexes. This makes it ideal for assessing rhythm, especially in detecting atrial activity and arrhythmias.
Can ECG leads be misplaced? What happens if they are?
Yes, ECG leads can be misplaced, and this can lead to misdiagnosis. For example, swapping right and left arm electrodes inverts Lead I and can mimic dextrocardia or lateral MI. Misplaced chest leads can mimic anterior MI or obscure true pathology. Proper training and adherence to guidelines are essential.
What are the 7 most important leads on ECG?
While all 12 leads are important, the 7 most clinically significant leads are often considered to be II, III, aVF, V1, V2, V5, and V6. These cover inferior, anterior, septal, and lateral walls, providing a robust diagnostic foundation for most acute cardiac events.
Understanding the intricacies of leads on ECG is not just for cardiologists—it’s a fundamental skill for any healthcare provider involved in cardiac care. From proper electrode placement to interpreting ST changes, each lead offers a unique window into the heart’s function. Whether you’re diagnosing a myocardial infarction, detecting arrhythmias, or utilizing AI-enhanced tools, mastering the 7 key leads on ECG empowers you to make faster, more accurate decisions. As technology evolves, so too does the role of ECG leads—but their core purpose remains unchanged: to listen to the heart’s silent language and respond with precision.
Further Reading: